Imagine being able to protect yourself from HIV with just two shots a year—no daily pill reminders, no stigma-inducing medicine bottles in your cabinet, just one injection every six months. That’s the promise of lenacapavir, a revolutionary HIV prevention tool that will soon be available for only $40 a year in 120 low- and middle-income countries (LMICs) starting in 2027.
RELATED: The Shot That Could End HIV: 100% Effective, 2 Injections a Year
Thanks to a groundbreaking partnership between Dr. Reddy’s Laboratories, Unitaid, the Clinton Health Access Initiative (CHAI), and Wits RHI, this injectable is set to reach millions of people who otherwise would not have had access so soon—or at such an affordable price.
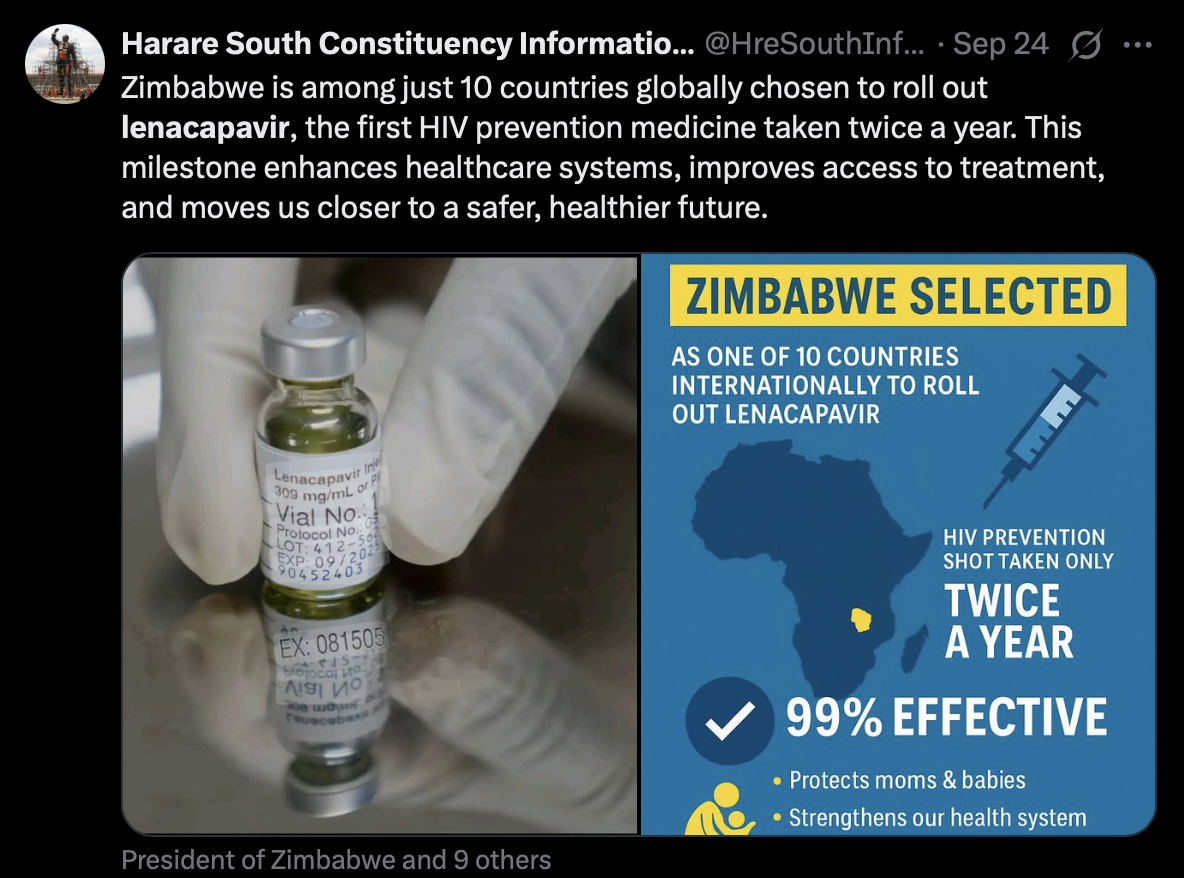
Originally developed by Gilead Sciences, lenacapavir (an antiretroviral treatment for HIV/AIDS) has already made headlines for its remarkable effectiveness: a single shot can protect someone from HIV for half a year. For those who find daily pre-exposure prophylaxis (PrEP) pills tough to stick with—whether because of stigma, side effects, or simply forgetfulness—this injection could be a game-changer.
Since 2010, global efforts have reduced new HIV infections by 40%, but 1.3 million people still contracted HIV in 2024. With a $40 per year price tag, experts believe lenacapavir could drastically lower those numbers. Why? Because cost and access have long been two of the biggest barriers to prevention. When prevention tools are both affordable and discreet, more people are likely to use them.

And the ripple effects go far beyond just protection. A cheaper, simpler prevention method means people may feel less afraid to get tested for HIV. The fear of judgment, of being “outed” at the pharmacy, or of not being able to afford treatment has kept many from seeking care. But with a twice-yearly shot that’s both affordable and stigma-free, more people may step forward to know their status, access treatment if needed, and stop the cycle of transmission.
Leaders around the world are already calling this agreement historic. Bill Clinton, co-founder of CHAI, called it a “fundamental shift in what’s possible for HIV prevention.” Meanwhile, Unitaid’s executive director Dr. Philippe Duneton emphasized that keeping the price in line with oral PrEP is critical for making sure people actually use it.
The deal is also significant because it closes the gap between high-income and low-income countries. Usually, new medicines take 10 years or more to reach LMICs at an affordable price. Here, we’re looking at access just under two years after high-income approvals—a speed unheard of in global health.
The injection still requires a short starter course of oral tablets—two pills on the first day and two on the second day of treatment—to get drug levels up to protective strength. But at a capped cost of no more than $17, the regimen remains well within reach.
For 20 years, Unitaid & @CHAI_health have worked together to make lifesaving medicines accessible. Today, that mission delivers again: a twice-yearly HIV prevention injection at just US$40/year for low- and middle-income countries.
Learn more: https://t.co/I6bs6uAjQ7 pic.twitter.com/WBEUQnwIOx
— Unitaid (@UNITAID) September 24, 2025
Looking ahead, experts are optimistic that this move won’t just reduce infections but will also chip away at the stigma surrounding HIV prevention. Imagine a future where protecting yourself from HIV is as routine—and as unremarkable—as getting a flu shot. That’s the kind of normalization lenacapavir could bring.
It’s a bold vision, but as global partnerships like this one prove, it’s possible. With affordability, accessibility, and stigma-free delivery all on the table, lenacapavir just might give the world its best shot yet at finally ending HIV. Let’s all simultaneously cross our fingers and hope for a better future with cheaper (and better yet free) medications.
REFERENCE: UNITAID